Non-Alcoholic Fatty Liver Disease: Global Scenario, Challenges, and Preparedness
Vol. 28, Issue 3 (September 2023)
 |
Akash Roy, MD, DM
Institute of Gastrosciences and Liver Transplantation
Apollo Multispecialty Hospitals
Kolkata, India
|
 |
|
Mahesh K Goenka, MD, DM, AGAF, FACG, FASGE,
FRCP (Glasgow & London)
Director and Head, Institute of Gastrosciences and Liver Transplant
Director, Medical Education
Apollo Multispecialty Hospitals
Kolkata, India
|
|
Introduction
Non-alcoholic fatty liver disease (NAFLD) has emerged as the most common and rapidly growing chronic liver disease globally with an estimated pooled prevalence of 32.4%. Additionally, an overall incidence of 46.9 cases per 1000 person-years.1 Regional variations remains a variable of the disease’s prevalence, with the highest prevalence in the Middle East and South America and the lowest in Africa.2 NAFLD is most commonly associated with the components of metabolic syndrome, the most common being obesity and diabetes mellitus.2, 3 In people with obesity and type 2 diabetes, NAFLD prevalence ranges as high as 50-70%.4, 5 Given these associations with obesity and type 2 diabetes and the exponential increment in these entities in conjunction with a globally aging population, the burden of NAFLD is projected to grow further.6 Because of such projected modeling of an incremental disease burden, developing strategies and policies to ensure adequate preparedness to combat the disease becomes imperative. Herein, we delve into a brief overview of the global scenario, challenges, and preparedness for tackling NAFLD.
Global Scenario
Over the past two decades, one of the key issues has been the variations in the reported prevalence of NAFLD, with differences arising out of geography, ethnicity, type of population studied, reporting, selection bias, and lack of uniformity in definitions. Albeit, the exponential evolution is reflected in the temporal change in NAFLD prevalence, which has increased by more than 50% from 25.26% (21.59-29.33) in 1990-2006 to 38.00% (33.71-42.49) in 2016-2019.7 The prevalence varies geographically, with the highest pooled prevalence being in Latin America (44.3%), followed by the Middle East and North Africa (MENA) (36.5%), South Asia (33.8%), Southeast Asia (33.1%), North America (31.2%,), East Asia (29.71%), Asia Pacific (28.0%), Western Europe (25.1%).7 In sync with the prevalence of NAFLD, the global prevalence of non-alcoholic steatohepatitis (NASH) is estimated to be 5.27%, with the highest prevalence being in Latin America (7.1%), followed by MENA (5.8%), South Asia (5.4%), Southeast Asia (5.3%), North America (5.0%), East Asia (4.7%) Asia Pacific (4.5%) and Western Europe (4.02%). When we look at subgroups, the prevalence of NAFLD goes up to 40%-60% in overweight and obese subjects and around 10% in lean subjects, with lean NAFLD being higher in Asians.8 NAFLD in people with diabetes appears to be most worrisome, with an overall global prevalence of 55.5% (95% CI 47.3-63.7) 37.3%, and 17% prevalence of NASH and advanced fibrosis, respectively.9 Lastly, beyond the adult population, NAFLD has also emerged as a growing problem associated with the pediatric population, with an overall pooled prevalence of 7.6%, which alarmingly increases to 34% in subjects with pediatric obesity.10
Challenges
Against the backdrop of the epidemiological burden, it is essential to identify the key challenges in the holistic management of NAFLD. The foremost challenge remains the need for more awareness regarding the entity and its relationship with poor metabolic health. While the impact of alcohol or viral hepatitis on liver health is well understood, the impact of lifestyle choices and metabolic co-morbidities leading to poor liver health in NAFLD has glaring gaps. Recent systematic reviews and surveys indicated a lack of sufficient communication between healthcare providers and patients, and obesity and diabetes are more concerning to the patients than NASH.11, 12 The lack of awareness and comprehension of the gravity of the problem transcends beyond patient-healthcare providers to overall governmental policy decisions. This is reflected in the need for additional focus on NAFLD in governmental health policies. The paucity of awareness is compounded by the variations in reported prevalence, lack of uniform diagnostic codes, good quality data on natural history with endpoints such as cirrhosis and hepatocellular carcinoma, and new controversies arising out of name changes to metabolic dysfunction associated fatty liver disease (MAFLD).13 The culminating point of these variations and lacunae in knowledge is the development of hurdles and stumbling blocks toward objective disease burden and outcome assessment. This in turn affects the development of uniform policy decisions in management. As the disease burden is of enormous magnitude, it also becomes imperative to develop appropriate referral pathways for specialist care from primary healthcare settings. There, however, still needs to be uniformity amidst guidelines recommended by various societies for appropriate referral pathways, which is again driven by demographic and epidemiological variations in different countries. Lastly, NAFLD being a hepatic reflection of metabolic dysregulation, there is an urgent need for concordance and consensus between different specialties, including primary care, endocrinology, cardiology, gastroenterology, and hepatology in terms of diagnosis, risk stratification, referral pathways, and management.14
Preparedness
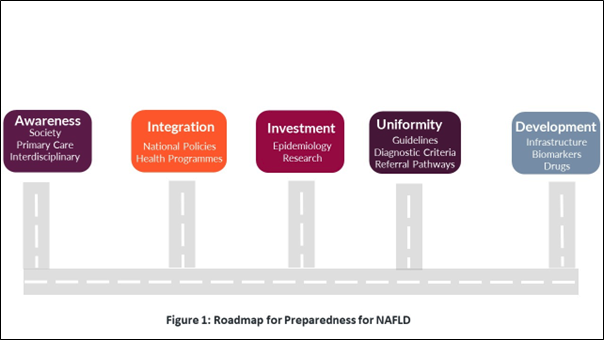
In the background of above-outlined burden and challenges, it becomes important to focus on strategies directed towards a holistic approach to NAFLD (Figure 1).
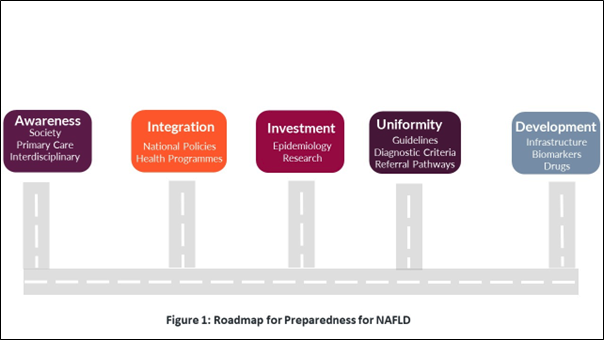
One of the crucial elements to address the challenges is to increase awareness amongst the public and health care providers to raise NAFLD to a similar pedestal as diabetes and obesity as markers of metabolic ill health. Furthermore, educating primary care providers about making appropriate diagnoses and ensuring effective clinical care pathways and referrals is important. In addition, interdisciplinary models of communication and management involving primary care, specialty, and subspecialty domains for uniformity in management need to be established.
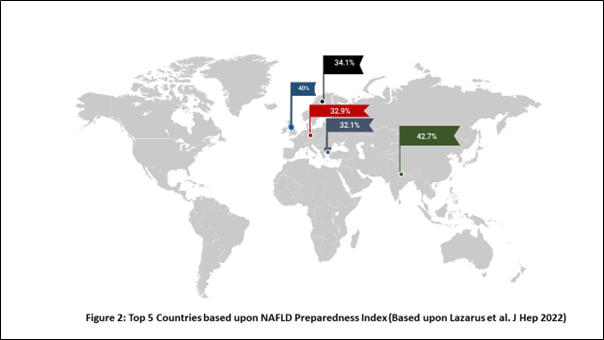
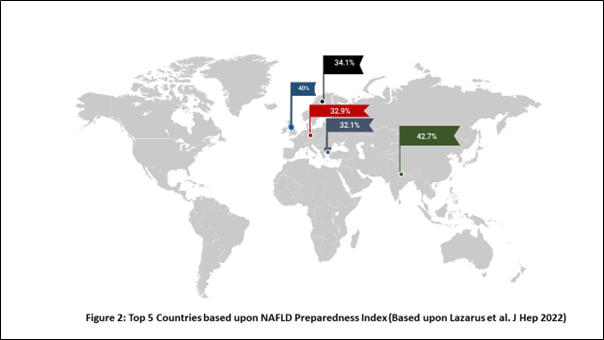
To achieve these core goals for holistic care, it becomes imperative to incorporate NAFLD as one of the non-communicable diseases and explicitly delineate the bidirectional relationship with diabetes mellitus, obesity, and other components of metabolic health. An effort to implement these strategies calls for adequate preparedness and planning. In 2019, a survey of 29 European countries was conducted addressing public health response strategies for NAFLD.15 Alarmingly, none of 29 participating countries had written strategies or action plans for NAFLD and only one-third reported having national clinical guidelines specifically addressing NAFLD. Only five countries reported having referral pathways, and only one-fourth had funded awareness campaigns.15 A follow-up survey assessed the preparedness index of countries based on four key domains of policies, guidelines, epidemiology, and care management.16 No countries were found to have yet attained a high level of preparedness. The United Kingdom (UK) scored best, although falling within the midlevel preparedness band, followed by Spain, and Denmark. While Spain scored highly in the epidemiology indicator category, UK was the only country that scored highly for care management.16 This concept was further expanded on a global scale involving 102 countries.17 The highest-scoring countries were India (42.7) and the United Kingdom (40), with almost a third of the countries scoring zero out of 100 (Figure 2).
One-third of the countries had national NAFLD clinical guidelines, while no country had a national or sub-national strategy directed specifically towards NAFLD.17 These findings indicate glaring deficiencies in preparatory strategies and policies addressing NAFLD. Such deficiencies call for urgent implementation of goal-directed measures across healthcare systems with a bottom-up approach starting from primary healthcare level up to subspecialty level care in the backdrop of specific national policies.
Conclusion
NAFLD is a major global public health challenge. Although several strides have been made in the understanding and management of the disease, its translation into acceptance as a public health challenge has several areas of deficiency. Globally countries lack appropriate preparatory strategies to combat the evolving epidemic of NAFLD. Holistic approaches involving increased awareness, infrastructure development, interdisciplinary collaboration and strategic action plans at national levels are urgently required for comprehensive care.
References
[1] Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2022;7:851–61. https://doi.org/10.1016/S2468-1253(22)00165-0.
[2] Lazarus J V., Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol 2021 191 2021;19:60–78. https://doi.org/10.1038/s41575-021-00523-4.
[3] Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62:S47–64. https://doi.org/10.1016/J.JHEP.2014.12.012.
[4] Portillo-Sanchez P, Bril F, Maximos M, Lomonaco R, Biernacki D, Orsak B, et al. High Prevalence of Nonalcoholic Fatty Liver Disease in Patients With Type 2 Diabetes Mellitus and Normal Plasma Aminotransferase Levels. J Clin Endocrinol Metab 2015;100:2231. https://doi.org/10.1210/JC.2015-1966.
[5] Lonardo A, Ballestri S, Marchesini G, Angulo P, Loria P. Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis 2015;47:181–90. https://doi.org/10.1016/J.DLD.2014.09.020.
[6] Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018;67:123–33. https://doi.org/10.1002/HEP.29466.
[7] Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 2023;77:1335–47. https://doi.org/10.1097/HEP.0000000000000004.
[8] Lu F Bin, Zheng KI, Rios RS, Targher G, Byrne CD, Zheng MH. Global epidemiology of lean non-alcoholic fatty liver disease: A systematic review and meta-analysis. J Gastroenterol Hepatol 2020;35:2041–50. https://doi.org/10.1111/JGH.15156.
[9] Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol 2019;71:793–801. https://doi.org/10.1016/J.JHEP.2019.06.021.
[10] Anderson EL, Howe LD, Jones HE, Higgins JPT, Lawlor DA, Fraser A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis 2015. https://doi.org/10.1371/journal.pone.0140908.
[11] Ng CH, Lim WH, Chin YH, Yong JN, Zeng RW, Chan KE, et al. Living in the non-alcoholic fatty liver disease silent epidemic: a qualitative systematic review of patients’ perspectives. Aliment Pharmacol Ther 2022;56:570–9. https://doi.org/10.1111/APT.17121.
[12] Cook NS, Nagar SH, Jain A, Balp MM, Mayländer M, Weiss O, et al. Understanding Patient Preferences and Unmet Needs in Non-alcoholic Steatohepatitis (NASH): Insights from a Qualitative Online Bulletin Board Study. Adv Ther 2019;36:478. https://doi.org/10.1007/S12325-018-0856-0.
[13] Fouad Y, Dufour JF, Zheng MH, Bollipo S, Desalegn H, Grønbaek H, et al. The NAFLD-MAFLD debate: Is there a Consensus-on-Consensus methodology? Liver Int 2022;42:742–8. https://doi.org/10.1111/LIV.15197.
[14] Ando Y, Jou JH. Nonalcoholic Fatty Liver Disease and Recent Guideline Updates. Clin Liver Dis 2021;17:23–8. https://doi.org/10.1002/CLD.1045.
[15] Lazarus J V., Ekstedt M, Marchesini G, Mullen J, Novak K, Pericàs JM, et al. A cross-sectional study of the public health response to non-alcoholic fatty liver disease in Europe. J Hepatol 2020;72:14–24. https://doi.org/10.1016/j.jhep.2019.08.027.
[16] Lazarus J V., Palayew A, Carrieri P, Ekstedt M, Marchesini G, Novak K, et al. European “NAFLD Preparedness Index” - Is Europe ready to meet the challenge of fatty liver disease? JHEP Reports Innov Hepatol 2021;3. https://doi.org/10.1016/J.JHEPR.2021.100234.
[17] Lazarus J V., Mark HE, Villota-Rivas M, Palayew A, Carrieri P, Colombo M, et al. The global NAFLD policy review and preparedness index: Are countries ready to address this silent public health challenge? J Hepatol 2022;76:771–80. https://doi.org/10.1016/J.JHEP.2021.10.025.