Telementoring for the Training of Flexible Endoscopy in Resource Limited Situations
Volume 28 Issue 4 (December 2023)
 |
Sandie Thomson, ChM, FRCS (Ed & Eng), FRCP(Ed),
MWGO
Emeritus Professor, Surgical Gastroenterologist
University of Cape Town
South Africa |
| |
|
 |
Chris Hair, MBBS BSc, FRACP, EGCOB, FGESA
Associate Professor, Gastroenterologist
Epworth Healthcare, Victoria, University Geelong
Fiji National University
Australia |
| |
|
 |
Srisha Hebbar, MBBS, FRCP
Consultant Gastroenterologist and therapeutic endoscopist
Endoscopy clinical lead
Clinical Director (specialised medicine)
Director of Stoke regional endoscopy course centre
University Hospital of North Midlands
United Kingdom |
| |
|
 |
Sabina Beg, MBBS BSc, PhD
Consultant Gastroenterologist
East and North Hertfordshire NHS Trust
United Kingdom |
| |
|
| |
|
Introduction
Telemedicine is an overarching term that encompasses all aspects of the use of information and communication technologies for the provision of medical health services at distant sites. It has come to the forefront during the COVID-19 pandemic which has focused development of platforms for patient care and the education and training of medical professionals. In the past, the application of telemedicine has seen significant growth among healthcare personnel. In 2020, the European telemedicine market was valued at $10.6 million.1
The focus of this review is to provide a background to the development and specific considerations related to the educational and ethical challenges posed by telementoring. Telementoring can be defined as the real time (synchronous) interaction using information and communication technology to teach or train medical health care providers procedural skills at the distant locations. This approach has been used by several procedural medical disciplines. The review will outline the history of telementoring, the basic technical tenets its ethical use and the potential application to train individuals in flexible endoscopy in under resourced environments.
Telementoring can be used to train relative novices in standard procedures, upskill experienced individuals or to train individuals on new equipment and novel techniques. The origin of medical telementoring is well established in the surgical specialties. They have coined a variety of terms of varying definitions which are valuable when discussing this modality of telemedicine.2 Teleproctoring, verbal guidance via a live feed by an expert to a trainee, is considered by many to be synonymous with telementoring. Telestration, the enhancement of the interaction by allowing the expert to indicate or draw on a live feed during a procedure, is increasingly combined with teleproctoring. The adoption of telementoring, teleproctoring and telestration by the gastrointestinal endoscopy community has lagged behind the surgical disciplines and its use has been confined to a few enthusiasts who have largely focused on proof of concept.3, 4
History
The first application of telementoring was in-house and occurred in 1996 using a dedicated T1 line for signal transmission.5 Two years later ophthalmologists telementored endoscopic laser-assisted dacryocystorhinostomy from Hawaii to the Philippines using ISDN transmission rates of 128 kilobytes per second.6 Since these pioneering days, the technology has moved forward with the use of high bandwidth videoconferencing, internet, and satellite transmission.
The adoption of telementoring or teleproctoring in the surgical disciplines was the subject of a systematic review reported in 2019.7 In this review they analyzed 66 studies. They concluded that telementoring has a similar safety and efficacy profile as on-site mentoring and that technological advances to improve remote connectivity would also aid the uptake of telementoring on a larger scale. The cheapest available was reported to cost $2750 (American dollars).8 This was a self-created system and is therefore limited to those surgeons with both the drive and technological abilities to replicate the system. The most expensive required an initial cost range of $50,000-$80,000 without taking into account yearly expenses.9
The first use of telementoring for any endoscopic procedure was reported for ERCP in endoscopy in 2013.3 Since then, the endoscopy literature has been dormant with a recent review on telemedicine in gastroenterology, devoting only one paragraph on telementoring.10 This dormancy was recently awakened by Dr. J. Waye who connected with a tech-savvy surgeon to set up the telementoring of a variety of endoscopy procedures. The procedures ranged from diagnostic and biopsy procedures to basic interventional procedures typified by variceal band ligation.4
Technical considerations
The key elements are video and audio capture from the trainee and mentor sites that are connected through an interface software program that enables transmission, recording and archiving, of minimal access procedures across a variety of interventional disciplines. 11, 13 These feeds can then be recorded and archived for educational interventions, future audit and potentially for medicolegal purposes. Additionally, these live or recorded feeds for audit by monitoring[CB1] [ZB2] of performance indicators, for medicolegal purposes and more importantly as an educational adjuncts for proceduralists, trainees, and the first step in enabling telementoring.
Bandwidth and latency are potential hurdles to effective telementoring. The amount of delay, connection stability, and integrity of the experience relies on an adequate bandwidth with minimal latency.14 To provide minimal latency times, bandwidth, known as the rate of data transfer between two points, should be sufficient. Bandwidth usage varies depending on video compression, image quality level, scene complexity, video resolution, and frame rate per second (FPS). Previously, bandwidth speeds depended on the type of data connection, distance of data transfer and overall traffic in the circuit. Currently with 5G, bandwidth speeds have reached 1Gb/s allowing short latency times and almost instant replay of the video transmission.15 However, improvements in video compression and transmission means that even with low to moderate bandwidth high quality transmission can be achieved.16
Transmitting and recording procedures can also pose challenges as the integration and manipulation of video sources (external cameras, views from flexible endoscopes, fluoroscopy, and ultrasound) are required to ensure consistent and optimal image quality, particularly for telementoring. 12, 13, 14
There are a variety of commercial devices that have been developed for specific purposes and companies that offer a specific software/hardware integration, with or without virtual tools that can improve educational aspects, particularly for telementoring. These include GoPro, Proximie, SWIS Surgical Video and SurgiCams[ZB3] [ZB4] . 17-19 Commercial entities often use low bandwidth internet connectivity, and encrypted web servers for bi-directional audio-video relay. However, these are costly, as are audio visual production companies to manage live transmissions. These costs act as a deterrence in the use of these products in resource-restricted healthcare environment. There is a paucity of systems developed using standard low-cost hardware and open-source software. 4, 12-14
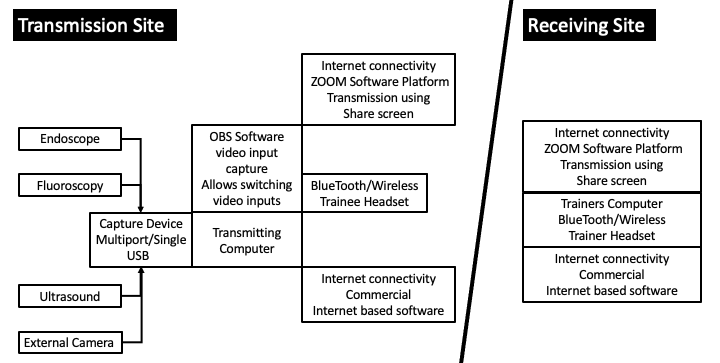
Figures 1 and 2 illustrate the principles of video audio capture and transmission, using either low cost equipment or a commercial platform. Figure 1.
Figure 1. Video and audio capture for transmission resource limited settings The video image is most simply captured by a DVI output from the stack to HDMI input to the capture card. This requires a reasonable computer or laptop with Open Broadcast Software (Open source software) installed. Audio is best transmitted by a wireless headset and microphone. The OBS window can be used for static image acquisition, recording, streaming, and on screenshare platforms (Zoom, Teams, Skype).
Figure 2.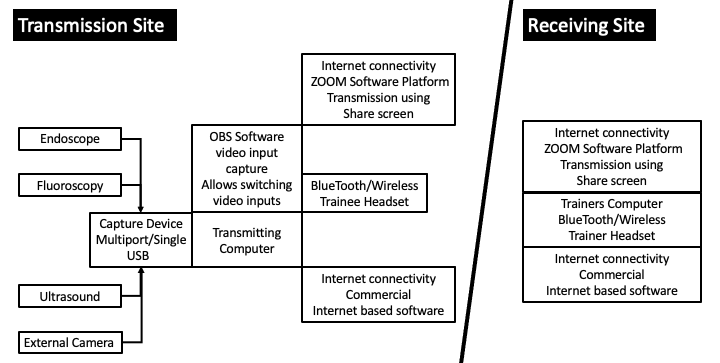
Figure 2. Telementoring Setup Telementoring setup for transmission and receiving sites. Capture software such as OBS allows integration of multiple inputs with varying picture in picture formats. Transmission site is more complex and stable internet connection is essential. Commercial software platforms such as Proxime have integrative telestration alternatives.
Implementation challenges
Having dealt with the technical feasibility and cost aspects of telementoring, there are several challenges to the implementation of telementoring in gastrointestinal endoscopy, particularly in low resourced settings.20, 21 The biggest challenges are the educational value and the situational and ethical considerations of remote training.
Educational principles
Telementoring in endoscopy has not been well adopted when compared to surgery, as recently illustrated in a study of ERCP practitioner attitudes.23 They showed user attitude towards widespread adoption of teleguidance in endoscopy as not positive for various reasons. These reasons include cost, time factor, technological and administrative issues and the complexity of remote mentoring of advanced in vivo procedures. However, telementoring has been trialed in a small study and has shown to improve the success of ERCP in low volume center.3 In this study, the cannulation rate of ERCP improved following remote mentoring, probably indicating that the low volume center gained from the experience and support of the high volume center.
For this to be replicated, it is important that the trainers involved in telementoring are not only highly skilled endoscopists, but are also great trainers. Trainers should be able to deconstruct and verbalize each step of the procedure and have good non-technical skills. There should be a form of interaction between the trainee and trainer before the commencement of the training.24 This interaction can be best conducted in person with a site visit or visits to the mentees institution and procedural environment. These visits not only help to establish a good rapport and working relationship, but can foster good listening skills and be used to address technical logistics.
One on the most unique aspects of telementoring is there is no concept of “take over the scope.” This creates difficulty for the remote trainer when the trainee does not understand, or cannot execute the commands, despite trying to follow the instructions. This can lead to non-completions or result in a complications, which may be demoralizing and have medicolegal implications.
Vivo remote training works best when the endoscopist is competent in the procedure but wants to improve certain specific techniques. These techniques include large balloon dilatation or fistulotomy in ERCP or wanting to learn better techniques to improve the speed of dissection. It can also be used for safe usage of newer accessories by competent endoscopists. For novice endoscopists, remote mentoring by a highly skilled trainer is still feasible on animal models, in vivo live anaesthetized pigs, or simulation-based training. This was successfully demonstrated in a small study of telementoring for ESD using live anaesthetized pigs.25
Remote video mentoring should ensure that it does not compromise the competency and skill development of clinicians. It is crucial to establish standardized protocols for remote mentoring, including assessments, evaluations, and ongoing feedback mechanisms to ensure that learners receive comprehensive training and develop the necessary skills. These educational principles and caveats are obviously important as we embark on the telementoring journey for flexible gastrointestinal endoscopy. However, it is equally important that we evaluate our efforts meaningfully and show, as the surgeons have done, that these methods works and can be further developed.26, 27 Only in this manner can we encourage the use of technology and develop the educational skills necessary for its use so we can improve endoscopic proficiency worldwide.

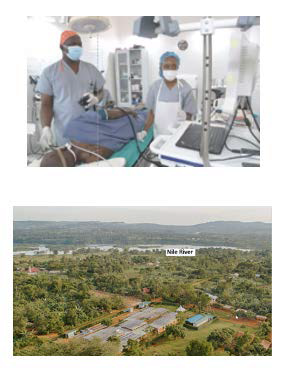
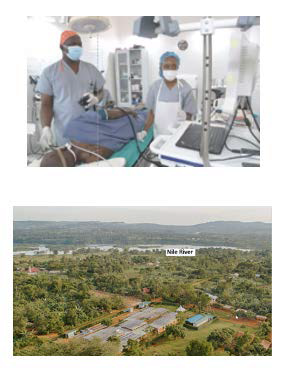
Figure 3. Live telementoring Illustrates a live telementoring session from Dr. Waye in New York to Dr. Joseph Okello Damoi and his nursing assistant Winfred Nannozi at Kyabirwa Surgical Center in Jinja, Uganda where he mentors on a variety of diagnostic andinterventional endoscopy procedures (with permission of Dr. Waye).
Ethical and medicolegal aspects
It is important in our enthusiasm to implement telementoring that we do not forget the medicolegal and ethical implications that are somewhat uncharted. The convergence of technology and medical education has led to new considerations. Remote video mentoring falls within the broader realm of telemedicine and telehealth. It is important to consider the legal frameworks and regulations specific to telemedicine in each jurisdiction, both nationally and internationally. Compliance with applicable telemedicine regulations, such as patient-doctor relationship guidelines, licensure requirements, and reimbursement policies are essential for telementoring to be conducted legally and ethically.
As telementoring gains traction as a method for teaching endoscopy, it is essential to be aware of the legal and ethical aspects specifically posed by this innovative approach. Unlike traditional in-person endoscopy training, remote mentoring introduces an additional layer of complexity and potential risks. These risks not only include traditional procedural complications, but also transmission failures that includes patient confidentiality breaches related to medical history, data and images.
The primary ethical concern surrounding remote video mentoring in endoscopy is the impact on patient safety. Ensuring patient welfare should always be the top priority, and any method used for teaching endoscopy must prioritize patient safety above all else. Consequently, the cardinal consideration of ethical appropriateness of remote video mentoring should be assessed based on its ability to maintain or enhance patient safety.
Another important factor is the issue of informed consent and patient autonomy and privacy. Patients should be given a clear understanding of the remote mentoring process and must provide informed consent for their involvement in mentoring sessions.28 The process of informed consent must be adequately documented. Procedures should be put in place to protect the mentor, the mentee, and the patient. Liability issues should be addressed through clear agreements and contractual arrangements that delineate the responsibilities and potential liabilities of each party. Both the mentor and the mentee involved in telementoring must possess appropriate credentials and valid licenses to ensure compliance with the regulatory requirements of the jurisdictions in which they are operating. Despite advances, there remains significant challenges in licensing for tele-mentoring and telehealth across national and international boundaries.29
Compliance with relevant data protection laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or General Data Protection Regulation (GDPR) in Europe are all part of the equation. These regulations may not exist in low- or middle-income countries (LMIC) and it is imperative when telementoring in these countries that the video communication channels are secure, and patient information remains confidential throughout the mentoring process.30, 31 Ethical responsibility also lies in the educational value of telementoring which should be equivalent or superior to the provision of traditional training and for continuing education and lifelong learning activities.
Conclusion
Telementoring is an underused but potentially transformative tool in the flexible gastrointestinal endoscopy training armamentarium. This has the potential to deliver high-quality bespoke training, with the ability to reach remote regions with minimal financial cost and carbon footprint. As with all technology, harnessing its true potential relies on understanding how it can be usefully applied to real life situations. Telementoring relies on understanding the technical abilities of the mentee and the expertise of the mentor. This modality is subtly different to traditional proctorship and therefore requires and adaptation of technique to compensate for the lack of nonverbal communication and ability to demonstrate hands on. In practice it is likely that a combination of both face to face and telementoring provides the most effective and safe model of training.
Further, consideration needs to be given to ethical and medicolegal implications of giving remote audio visual mentoring. Ethical guidelines and standards should be established to ensure that this emerging practice aligns with the highest moral principles and contributes to the overall improvement of clinical education while prioritizing patient wellbeing. Balancing patient safety, informed consent, and competency development are essential considerations. These factors go hand-in-hand with adherence to evolving legal frameworks that govern this type of medical practice.
Telementoring has hurdles to overcome in order to be able to disseminate the technique. By addressing the problems, we believe this can enhance the training of flexible endoscopy globally for both diagnostic and advanced therapeutic procedure. This has the potential to foster local talent, particularly in resource limited settings, and in turn empower local and regional service development.
References:
- Intelligence M: Global telemedicine market - growth, trends and forecasts 2021–2026.: http://www.mordorintelligence.com/ industry- reports/global- telemedicine- market- industry.
- Ayoub CH, El-Asmar JM, Abdulfattah S, El-Hajj A. Telemedicine and Telementoring in Urology. Frontiers in Surgery. 2022: 9 doi: 10.3389/fsurg.2022.811749
- Påhlsson HI, Groth K, Permert J, et al. Telemedicine: an important aid to perform high-quality endoscopic retrograde cholangio-pancreatography in low-volume centers.
- Waye JD, Marin ML, Damoi JO et al. Remote training in flexible gastrointestinal endoscopy VIDEOGIE 2021;6(10):439
- Moore RG, Adams JB, Partin AW, et al.Telementoring of laparoscopic procedures: initial clinical experience. Surg Endosc. 1996;10:107-110. https://doi.org/10.1007/BF00188353.
- Camara JG, Rodriguez RE. Real-time telementoring in ophthalmology. Telemedicine J. 1998;4:375-377. https://doi.org/10.1089/tmj.1.1998.4.375.
- Erridge S, Yeung DKT, Patel HRH and Purkayastha S. Telementoring of Surgeons: A Systematic Review. Surgical Innovation 2019:26(1) 95–111
- Gambadauro P, Magos A. NEST (network enhanced surgical training): a PC-based system for telementoring in gynaecological surgery. Eur J Obstet Gynecol Reprod Biol. 2008;139:222-225.
- Singh S, Sharma V, Patel P, Anuragi G, Sharma RG. Telementoring: an overview and our preliminary experience in the setting up of a cost-effective telementoring facility. Indian J Surg. 2016;78:70-73.
- Fung BM, Markarian E, Serper M, Tabibian JH. Current Applications of Telemedicine in Gastroenterology. Am J Gastroenterol 2022;117:1072–1079. https://doi.org/10.14309/ajg.0000000000001761
- Saun TJ, Zuo KJ, Grantcharov TP. Video technologies for recording open surgery: A systematic review. Surg Innov. 2019;26:599-612. https://doi.org/10.1177/1553350619853099.
- Lazarus J, Thomson SR. Video transmission of urology surgeries: proof of concept in a resource-constrained environment African Urology 2022;2(2):60-64 https://doi.org/10.36303/AUJ.0035
- Shimizu S, Itaba S, Yada S et al. Significance of telemedicine for video image transmission of endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography procedures. J Hepatobiliary Pancreat Sci 2011;18:366–374
- Shimuzu S, Thomson S, Doyle G et al. Live surgery broadcast from Japan to South Africa: high-quality image transmission over a high-speed academic network. J Int Soc Telemed eHealth 2013;1(3):80-85
- Zheng J, Wang Y, Zhang J, Guo W, Yang X, Luo L, et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc. 2020;34:5172– 80. doi: 10.1007/s00464-020-07823-x
- Kumar KS, Kumar SS, N.Mohan N, et al . Effcient video compression and improving quality of video in communication for computer end coding applications Computer Communications. 2020:153;152-158
- Proximie Homepage [Internet]. Retrieved September 22, 2020, from https://www.proximie.com/ S.W.I.S surgical. (n.d.).
- S.W.I.S surgical. (n.d.). S.W.I.S. Surgical Video System [Internet]. Retrieved from https://swissurgicalvideo.com/
- Surgicams. (2020). Surgicams homepage [Internet]. Retrieved September 23, 2020, from https://surgicams. com/
- Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-24. https://doi.org/10.1016/S0140-6736(15)60160-X..
- Wachs JP, Kirkpatrick, AW and Tisherman SA. Procedural Telementoring in Rural, Underdeveloped, and Austere Settings: Origins, Present Challenges, and Future Perspectives Annu. Rev. Biomed. Eng. 2021;23:115–39
- El-Asmar JM, Labban M, El-Hajj A. Integration of aqua-ablation through telemetry: an alternative to onsite proctoring?. World J Urol. 2021;39:3473– 9. doi: 10.1007/s00345-021-03603-x
- Aminoff H, Meijer S, Arnelo U, Frennert S. Telemedicine for Remote Surgical Guidance in Endoscopic Retrograde Cholangiopancreatography: Mixed Methods Study of Practitioner Attitudes. JMIR Form Res. 2021;11:5(1)
- Sutton PA, Beamish Aj, Rashid S, et al. Attributes of excellent surgical trainers: An analysis of outstanding trainers Editorial. International Journal of Surgery. 2018:52;371-375.
- Yip HC, Uedo N, Lau LH, Hirata D, Sano Y, Chiu PW; Asian Novel Bio-imaging and Intervention Group (ANBIIG). Telementoring for endoscopic submucosal dissection in vivo training. Dig Endosc. 2023;35(1):140-145
- El-Asmar JM, Labban M, El-Hajj A. Integration of aquablation through telemetry: an alternative to onsite proctoring?. World J Urol. 2021;39:3473– 9. doi: 10.1007/s00345-021-03603-x
- Collins JW, Levy J, Stefanidis D, et al. Utilising the Delphi process to develop a proficiency-based progression train-the-trainer course for robotic surgery training. European Urology. 2019;75:(5)775-78. https://doi.org/10.1016/j. eururo.2018.12.044.
- Botrugno C. Telemedicine in daily practice: Addressing legal challenges while waiting for an EU regulatory framework. Health Policy Technol 2018;7:131–136
- Kruse CS, Williams K, Bohls J, Shamsi W. Telemedicine and health policy: asystematic review. Health Policy Technol. 2021;10:209–29
- Nittari G, Khuman R, Baldoni S, Pallotta G, Battineni G, Sirignano A, et al.. Telemedicine practice: review of the current ethical and legal challenges. Telemed J E Health. 2020;26:1427–37.
- Bonaci T, Herron J, Yusuf T, Yan J, Kohno T, Chizeck H. To make a robot secure: an experimental analysis of cyber security threats against teleoperated surgical robots. arXiv Preprint arXiv:150404339. 2015